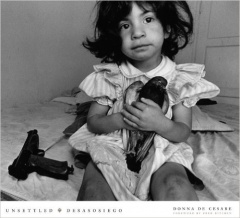
The Children of Central City
Rates of PTSD soar among Central City children,
yet state budget cuts prevent access to mental healthcare
On a Sunday night in Central City in 2014, Earl Watson pulled his car into a fast-food parking lot to pick up his 5-year-old son, Earl Jr., from his godmother. As Watson got out of his car, he saw a man and a woman arguing. Within seconds, the woman took out a gun and fired twice, dropping the man.
Watson’s son sat wide-eyed in his godmother’s vehicle just a few feet away.
“The guy’s friend runs to his car, starts searching in the trunk like he’s looking for a gun,” Watson said, describing the scene that followed. “She’s standing over the dude she shot, saying, ‘I told you.’ Her daughter is in her car saying, ‘Momma, come on, he’s got a gun, too.’ She had a car full of people, little kids and everything. It was crazy.”
Watson’s son was physically unharmed. But emotionally, he hasn’t been the same since.
“If a fire truck came through with the sirens, he’d come inside running,” Watson said of his son in the months after the shooting. “He’d be crying, hysterical. His nerves are real bad. He chews off the skin to his fingers.”
In Central City, one of New Orleans’ most crime-afflicted neighborhoods, Watson’s story is not an isolated occurrence. Many Central City children have been exposed to so much violence that they show evidence of post-traumatic stress disorder in rates higher than soldiers returning from war, according to recent studies.
Most of those children and their families, however, suffer with little help. A small patchwork of New Orleans schools, nonprofit groups and healthcare agencies are cobbling together support for traumatized children, but that reaches only a small fraction of the thousands in need.
Advocates place much of the blame in Baton Rouge: Former Louisiana Gov. Bobby Jindal eliminated a statewide mental health care program for children 5 years old and younger. More than five years later, Gov. John Bel Edwards made cuts to drastically reduce Medicaid-funded mental health services for children of all ages.
Michelle Alletto, deputy secretary for the Department of Health, said the decision was an unfortunate necessity given the state’s $300 million deficit at the time. Edwards values mental health care for children, she said, but it often falls victim to what many view as more pressing needs.
“You can physically see someone on dialysis. You can physically see someone in hospice. You can see some physical disability,” she said. “But it’s very hard to show people mental health. Prevention is a very difficult thing to sell.”
This lies at the heart of the problem, said Paulette Carter, president and CEO of Children’s Bureau of New Orleans, a nonprofit that provides trauma-related mental health services to young people and their families. Public officials, both past and present, have failed to grasp the seriousness of the psychological injuries suffered by these uncounted victims of violence, Carter said, in addition to the long-term benefits of providing treatment.
That won’t change, advocates argue, until officials – and the public in general – understand the devastating impact of violence-induced trauma on the most vulnerable of children – impoverished, black and living in the city’s most dangerous neighborhoods.
“We have to acknowledge the fact that kids are hurt,” Carter said. “It’s easier for people to not think about those awful things, because those are hard conversations. But we have all these kids hurting, and by not helping them or trying to understand, we’re traumatizing them even more.”
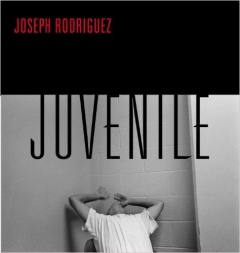
On the banks of Bayou St. John, just across from City Park in Gentilly, is the Youth Study Center, the city’s juvenile detention facility. At any one time, it holds up to 48 children under the age of 16. Of every 100 children who pass through it, 96 are black.
Social worker Heather Kindschy remembers visiting one of her first clients at the jail. He was 9 years old. She can still picture him, Kindschy said, this tiny child, crying out for his mother, swallowed up by the oversized cell. She asked if there was anything she could bring to make him feel better. His reply: a Spider-Man coloring book.
“It’s always alarming to us how small (they) are,” Kindschy said as her colleague at the time, Preet Samra, nodded in agreement. “And if they’re arrested, that means they’ve been booked, had their fingerprints taken, their mug shot taken, possibly their DNA harvested. What does that teach them?”

Kindschy is a licensed clinical social worker with the Louisiana Center for Children’s Rights, the public defense agency for juveniles. Samra served in the same capacity before taking a job earlier this year with the public defender’s office in Santa Clara, Calif. Their job is to support children and their families as they work their way through the legal process. This can include providing transportation to court, making sure they are enrolled in and attending school, or arranging mental health treatment, if needed. In their experience, mental healthcare is needed in nearly every case.
More than 90 percent of the children they represent have personally known someone who has been killed, Kindschy estimates, while a slightly smaller number have actually seen someone murdered. These traumatized children often act out or exhibit troublesome behavior. Yet far too often, the solution offered by adults is to punish or lock them up, even if the alleged crime is relatively minor, Samra said.
The 9-year-old Kindschy represented had been arrested for a status offense, something that was criminal only because of his youth, such as truancy or running away from home. Only 17 percent of children in the Youth Study Center last year were arrested for violent crimes, according to LCCR.
“It’s hard for us to get (parents) to understand what trauma does and how it can affect kids,” Samra said. “A lot of parents are like, ‘He doesn’t come home at night. I just can’t control him. He just needs to go sit at Youth Study for a few days, so he can learn a lesson.’
“I don’t know how many times I can say it. Jail is not the answer.”
The answer, experts say, lies in the field of mental health care. Therapeutic techniques, such as cognitive behavioral therapy, have proven to decrease symptoms of violence-induced mental health disorders by an average of 50 percent in the first three months of treatment, according to Dr. Michael Scheeringa, vice-chair of research with the Department of Psychiatry and Behavioral Sciences at Tulane University School of Medicine.
Cognitive behavioral therapy teaches children how to process their trauma while better regulating their thoughts and emotions through relaxation exercises and coping skills. Kindschy has seen these trauma-focused treatments at work. She remembers a young girl she represented who saw someone killed at a corner store near her home. After the shooting, the girl couldn’t walk near any corner store without suffering from severe anxiety attacks. Over time, and with the help of a therapist, she conquered her fears.
“It’s an exposure therapy. It’s really intense for kids. ‘Let’s sit down and talk about the worst day you ever had and let’s talk about it again and again and again.’ But, at the end, this girl was able to walk to the corner store and get a bag of chips,” Kindschy said.

Watson, whose son saw a man shot to death in the fast-food parking lot in Central City, arranged to have a therapist come to their home once a week. While his son continues to struggle emotionally, he is making progress, Watson said.
“I see E.J. sometimes shutting down. He gets quiet. I try to talk to him and he says, ‘I’m all right, daddy.’ But he’s getting better. I think it’s helping,” he said of his son’s sessions with the therapist. “Sometimes kids won’t open up to you, but they’ll open up to them and they might find out something we can’t. We’re just doing what we can, trying to keep him safe.”
In New Orleans, despite the overwhelming need, there are just a handful of organizations, outside of counseling in some schools, that provide trauma-focused, evidence-based therapies. These include the nonprofit Children’s Bureau of New Orleans and the state-run Metropolitan Human Services District.

Their efforts, however, are consistently undermined by state budget cuts and a lack of support among local leaders. Nearly a quarter of Metropolitan’s budget has been cut over the past eight years, and yet few people have risen to defend the agency’s mission, said its executive and medical director, Dr. Rochelle Head-Dunham.
“Look at the mayoral race. Did you hear anybody talk about mental illness as part of their platforms? Not a single one. And yet, they’re talking about all these (criminal) behaviors. Where do you think these behaviors are coming from?” Head-Dunham said.
Many traumatized children struggling with mental illness self-medicate, primarily with marijuana, to calm their nerves, Kindschy said. This puts them at greater risk for arrest, but for many it’s the only option given the state’s failure to provide mental health care for low-income families, she said.
“If you have money, if you have the means, if you have access to transportation, if you have really involved parents and you have trauma, it might not be that hard for you to be resilient and bounce back,” Kindschy said. “For other kids who have so many strikes against them and don’t have any of those protective factors, everything is more difficult.”

In June 2012, Peaches Keller’s brother was shot dead in Central City. Sixteen months later, her sister’s body was found inside an Algiers home. She had been “sliced up,” prosecutors said, strangled and beaten almost beyond recognition.
In the months that followed, Keller said her 8-year-old son Elijah, started having problems in school. He was becoming increasingly angry, accusing other children of talking about his deceased aunt. In his first few days at Good Shepherd Nativity School, he nearly got into two fights with classmates.
His mother knew he needed help coping with the losses — the entire family did, she said — so she contacted Ashley Hill, a therapist with Destined for a Change, a mental health clinic in Algiers.

Hill began visiting Elijah and his three siblings up to four times a week, both at his home and in school. They grew attached to her, Keller said, like she was a member of the family. Gradually, things started to get back to normal. Elijah was learning to better control his emotions.
Then Hill gave the Kellers some bad news. The state’s managed care organizations that oversee distribution of Medicaid dollars determined Elijah was no longer eligible for Hill’s services. He had stopped getting into fights at school and was now passing his classes; he was, in the eyes of the state, cured, Hill said.
After Hill stopped visiting Elijah, his grades once again plummeted while his behavior deteriorated.
“The school’s been having to call us for situations where he has been walking out of the class and doing all types of crazy stuff,” his mother said.
The Kellers were among the families affected when Edwards cut $49 million in behavioral health services from the 2017 budget. Faced with a $300 million deficit, the administration and legislators slashed higher education and health care, the two most-heavily funded government programs whose budgets are not protected by the state constitution and, therefore, frequently targeted for cuts.
To accommodate the $49 million cut, the state made eligibility requirements for some mental health programs more restrictive – leaving out the Kellers and many families like them.
Alletto, the health department’s deputy secretary, acknowledged that there will be “families across the state that could potentially experience a disruption in the service from a provider they’ve been seeing for a while and are familiar with.”
Hill worries about the long-term effects such disruptions will have on Elijah’s recovery, and other children just like him.
“I’ve seen how it plays out,” she said of untreated trauma. “I work with a lot of adults and they have trouble holding down a job or maintaining a stable household. The emotional trauma they experience still has major influence.”
The first step in providing help to children is to acknowledge that bad things happen to them, says Paulette Carter, president and CEO of Children’s Bureau of New Orleans, a nonprofit that provides trauma-related mental health services to young people and their families.
Paulette Carter operates Children’s Bureau of New Orleans, one of the largest providers of trauma-focused mental health care for children in Southeast Louisiana. The nonprofit has been around for more than 125 years, dedicated to waging “war against all the enemies of little children.”
In the city’s poorest neighborhoods, there is perhaps no greater enemy of children than the trauma they suffer from being exposed to violence and poverty, Carter said.
“I had a kid who came in who had bruises all over from being whipped with an electrical cord. Yeah, there is a reason why this kid is acting out,” she said.
Children’s Bureau provides therapy and crisis intervention services to more than 3,000 children and their families per year. It also provides mental health treatment to young people at the Youth Study Center through a federal grant from the Crime Victims Fund. The pilot program has proven to be a success, with 89 percent of the children showing a reduction in their symptoms.

Carter, however, doesn’t know how much longer they will be able to operate. Children with the greatest need are all on Medicaid – which accounts for 75 percent of Children’s Bureau’s budget – but reimbursement rates are so low and cover so few services, it makes it nearly impossible to stay in business.
Louisiana annually spends an average $1,933 per child in Medicaid, the fourth lowest in the country, according to the Kaiser Family Foundation. The state’s Medicaid plan pays for an hour-long counseling session, Carter said, but it doesn’t reimburse clinicians for the bulk of services associated with treating children, including case management, transportation to and from homes and schools, consultations with parents, and associated paperwork.
“My least experienced staff are working with my most complex cases because that’s all I can afford,” Carter says. “I can’t afford to hire a licensed clinician that has 10 years of experience. I can only hire ones right out of school or (who) have only had a year or two of experience.”
Hiring is also hard when most experienced clinicians can make more in private practice. Carter recently advertised a post with a $50,000 salary. In two weeks, not a single qualified person applied.
Alletto acknowledges the current set-up makes it more difficult on providers.
“When you can’t pay adequately, it becomes harder to push quality and change the way you practice,” she said. “Louisiana is really behind the curve in developing a behavioral health network."

Louisiana’s substandard mental healthcare services for traumatized children can be traced, in large part, to Jindal’s decision as governor six years ago to eliminate the state-operated Early Childhood Supports and Services program, Carter said.
The program had 10 sites across the state, including one in New Orleans, that provided mental healthcare to children under the age of 6 who had been exposed to violence and were at risk of developing mental illnesses. The program, founded in 2002, also provided support services for their families.
Jindal questioned the effectiveness of these services and claimed they could be better delivered by pediatricians and nonprofits. Pediatricians, however, are not trained to diagnose or treat trauma, and cash-strapped nonprofits can’t afford hiring early childhood specialists, said Dr. Mary Margaret Gleason, formerly a co-clinical director with the program and currently an associate professor of psychiatry at Tulane University. As a result, mental health care for children under 6 nearly disappeared in New Orleans.
Joy Osofsky, professor of Pediatrics and Psychiatry at LSU Health Sciences Center, operates one of the last remaining mental health programs in the city that treat children under the age of 6. The decision to end ECSS is representative of an overall undervaluing of the work they do and the children they serve, who are nearly all poor and black, she said.
“Every time there is a shooting you’re going to hear, ‘We need more mental healthcare.’ That will last for about three days,” Osofsky said. “For too long, there was the idea that young children wouldn’t notice trauma, that it wouldn’t have an effect and they would just get over it. The evidence is just the opposite.”

While Louisiana has cut mental health services for children, some other states are adding it. Wisconsin, which ranks second to last in per-child Medicaid spending, announced a $17 million expansion this year for mental health and substance abuse treatment that would increase pay rates for medical professionals who treat low-income people, including children.
North Carolina has also revamped its Medicaid system, paying providers about $13,000 for the duration of a single child’s treatment, as long as they are utilizing evidence-based practices, says Dr. Dana Hagele, co-director of the state’s Child Treatment Program. This amount is based on an actuarial table of what it costs to provide quality care while operating a business in a way that ensures it doesn’t go bankrupt. Given the cost-benefit analysis, Hagele says it wasn’t difficult to convince state officials to make the change.
“If just 15 kids avoid a year in a psychiatric facility because they got services from our program, it would pay for the entire program,” Hagele says. “That’s just 15 kids a year. There is a cost savings. The math is a no-brainer.”

It’s time Louisiana began to look at mental healthcare for children exposed to violence in the same way: not as a luxury, but as a vital necessity, a sound investment in the future of its children, and a prudent expenditure of public dollars, Gleason said.
“Outcomes across the board improved for people who got this early intervention,” Gleason said. “It doesn’t cost that much to do the kind of services we’re talking about in young children. It provides the power of changing a life and decreasing the financial burden on society.”
Mental health providers point to studies that show the benefits of providing trauma-focused therapy. There’s the Heckman Equation by James Heckman, a professor of Economics at the University of Chicago and a winner of the Nobel Memorial Prize in Economics. It found that early childhood care from birth to age 5 has a 13 percent return on investment.
Conversely, a report from the Centers for Disease Control and Prevention estimated the lifetime public cost for a child exposed to violence, abuse or neglect and who does not receive adequate mental health treatment is $210,012. This reflects the costs of healthcare, welfare and the criminal justice system, in addition to future losses of productivity.
For example, in research conducted in New Orleans, 42 children at Lawrence D. Crocker College Prep screened positive for lifetime PTSD. If those 42 children did not receive adequate treatment, the CDC estimates the cost to society would rise to $8.8 million.

James Bueche, deputy secretary for the Office of Juvenile Justice, says that nearly 100 percent of the young people held in state juvenile detention facilities experienced at least one trauma that has resulted in mental health problems.
The state spends more than $53,000 a year to incarcerate one minor. Bueche said he would rather see that money go towards prevention so these boys and girls never reach any of the facilities he oversees.
“That’s where you are going to get the biggest bang for your buck, not waiting until you’re having to pay $200, $300 a day,” Bueche said.
A frustrated Carter said this is what she and others have been saying for years, but too much of their time is spent “trying to convince people that (trauma) is an illness like any other illness that needs to be treated.”
What is society’s resistance to accepting trauma as a real threat, she asks, communicating to those children who desperately need help and can’t find any?
“The message they often get is, ‘You’re not strong enough and you don’t matter enough for us to care,’” Carter said. Her organization, she added, “tries to say, ‘You do matter and we’re going to fight for you and be here for you. But you also are strong enough to get through this and to be who you want to be.’”
- Previous Section
The Science of Trauma - Next Section
Malachi's Story